The myeloproliferative neoplasms (MPN) are a class of incurable diseases that may have great effects on patients. Though the incidence (number of people that get the disease) is low, patients generally live for a long time. According to the Surveillance, Epidemiology, and End Results (SEER) program of the National Cancer Institute, the high range estimate is that ~20,000 people get an MPN each year and there are ~295,000 people living with an MPN in the United States. Since these diseases can initially cause no symptoms in patients, and because of the long course of the disease, it is likely that many people with an MPN remain undiagnosed. Patients living with MPNs often have symptoms that affect their quality of life. In addition, MPNs often progress to a more aggressive acute leukemia that is usually lethal. Therefore, there is a great unmet need to find a cure for this set of diseases.
The World Health Organization considers a number of diseases to be MPN, but the ones most often classified as MPNs are the Philadelphia chromosome negative MPNs: polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF). These all share some overlapping characteristics, especially the presence of mutations in either JAK2, CALR, and/or MPL. Importantly, these MPNs do not have the chromosomal translocation producing the BCR/ABL fusion gene that is indicative of the Philadelphia chromosome positive MPN chronic myeloid leukemia (CML). Therefore, the presence of mutant JAK2, CALR, or MPL is generally indicative of a classical MPN, and at present, mutant JAK2 is part of the standard diagnostic criteria. MPNs are typically diagnosed after the age of 50, with most patients being in their 60s and 70s. However, there are rare cases of MPNs in younger patients.
Are you a Patient or Caregiver? Click here for our free informational booklet on MPN.
Disease subtypes
Polycythemia vera
PV is characterized primarily by an increase in red blood cells. Patients may present with headaches, itching, bleeding disturbances, and/or blood clots as well as other symptoms. “Polycythemia” refers to an increase in red blood cells, which may be the result of numerous conditions; therefore, care must be taken to appropriately diagnosis those presenting with increased red blood cells. Since 95% of all PV patients have a specific mutation in JAK2 (JAK2 V617F), the presence of elevated red blood cells (as measured by hemoglobin levels) and the presence of mutant JAK2 V617F are the diagnostic criteria for PV. The few patients suspected of having PV but without JAK2 V617F should be definitively diagnosed at a center specializing in MPNs.
At present, there is no cure for PV (outside of hematopoietic stem cell transplant, which has significant complications, especially for older patients). Therefore, treatment seeks to control symptoms. The most significant complication of PV is thrombotic events-blot clots in various places that may cause heart attack, stroke, or other complications such as liver failure. Therefore, a major goal of treatment is to reduce blood cell numbers to decrease the risk of these complications. Patients who are considered low risk (younger than 60 with no history of blood clots) may be treated with aspirin as well as phlebotomy, which may reduce some symptoms. (Patients should consult their physician before taking aspirin, as there are some patients for whom this may exacerbate their specific symptoms). For patients with more symptoms or with higher risk disease, specific drugs to reduce blood counts may be used. The most common drug is hydroxyurea, which is generally safe and most patients respond well. An important consequence of hydroxyurea is a reduction in the risk of thrombosis. For those that do not respond to hydroxyurea, the JAK2 inhibitor ruxolitinib provides relief.
The median age at diagnosis is 60. The 5 year survival rate for PV patients is 85%, which is close to the expected survival of age- and gender-matched healthy people. However, at 25 years post-diagnosis, the expected survival is only 20%, which compares unfavorably to the 55% survival rate for healthy, matched people.
Essential thrombocythemia
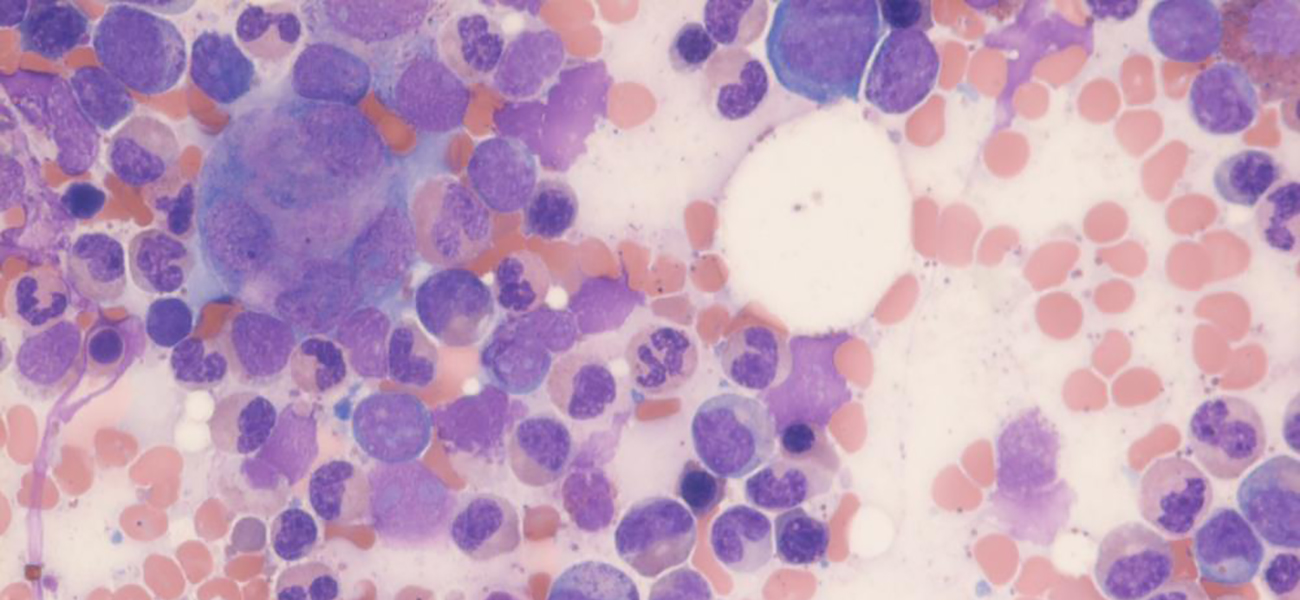
ET is characterized mainly by an increase in platelets. Patients may present with symptoms such as vision changes and headaches as well as enlarged spleen, thrombosis, and bleeding disturbances. Most patients who have an increase in platelets do not have ET, but may have an infection, inflammatory disorder, or other malignancy, thus a differential diagnosis is important. Over 80% of ET patients have mutations in the JAK2, CALR, or MPL genes. Therefore, an elevated platelet count together with a mutation in one of these genes is diagnostic for ET if other diseases are ruled out. Since platelets are produced from the blood cell type called megakaryocyte, patients will often have elevated megakaryocytes in the bone marrow, many of which are malformed.
Like PV, the major problems associated with ET are thrombotic events and bleeding, with thrombotic events contributing to mortality. Those with higher risk disease (older than 60, prior thrombotic events, very high platelet counts) are treated with hydroxyurea or interferon-a to reduce cell counts and therefore reduce the chance of a thrombotic event. Clinicians may use a watch and wait strategy for lower-risk patients. Hematopoietic stem cell transplant may be considered, especially for younger patients.
The median age at diagnosis if 50-60. The 5 year survival is equivalent to matched, healthy people whereas the 25 year survival is 40% compared to 55% for healthy, matched individuals.
Primary myelofibrosis
PMF is characterized by abnormalities in various blood cell types as well as fibrosis-the accumulation of extracellular fibers in the bone marrow. Though the name indicates that fibrosis is a primary component of the disease, it is actually a secondary effect of malfunctioning megakaryocytes that appear to secrete factors that cause non-malignant fibroblasts (connective tissue cells) to produce more collagen that is deposited as fibers in the bone marrow. This is the only cancer named for a secondary effect of the disease.
Patients may present with fatigue, weight loss, fever, and night sweats. Because the spleen is usually enlarged, there may be discomfort or fullness on the upper left side. Diagnostic criteria include anemia, enlarged spleen, malformed red blood cells, immature cells in the blood, and an increase in megakaryocytes that are malformed are found in the bone marrow. In addition, whereas PMF should not have BCR/ABL, ~95% of patients have mutations in JAK2, CALR, or MPL. A challenge with PMF is that there may be a pre-fibrotic stage where the collagen fibers are not seen in the bone marrow. This disease can resemble ET, and so it is imperative to be diagnosed by an experienced clinician to determine if the patient has ET (a less aggressive disease) or PMF (a more aggressive disease).
The only cure for PMF is hematopoietic stem cell transplantation, which may be considered for younger patients with a more aggressive disease. Some patients show no symptoms and may not require treatment for years. Treatment typically seeks to reduce the symptoms such as anemia and enlarged spleen. A number of drugs may be used for these symptoms, with a common drug being the JAK2 inhibitor ruxolitinib. This drug does not cure PMF, but it greatly reduces the symptoms, especially spleen size, as this can be a major impediment to patients.
The median age at diagnosis is between 65 and 70 years old. In contrast to PV and ET, PMF has a high mortality rate. At 5 years, the survival rate is 55% compared to 90% for matched, healthy people. At 25 years the expected survival in healthy people is 55%, whereas it is ~10% for PMF patients. Even though there is a roughly similar yearly incidence of new diagnoses for ET, PV, and PMF patients, only ~5% of those currently living with an MPN are PMF patients.
Progression
A major concern of MPN patients is progression to a more aggressive disease. Both ET and PV are generally less aggressive forms of cancer, and they both may progress to myelofibrosis. The names may be “post ET MF” or “post PV MF,” or the name may be “secondary MF.” However, “secondary MF” may also be the name for myelofibrosis that is secondary to other diseases that are unrelated to MPNs. Post ET MF and post PV MF appear to behave clinically like PMF. However, recent genetic analyses demonstrate some mutational differences between primary and secondary MF. The significance of these findings requires more research and analysis of greater numbers of patients, but these findings suggest that there may be some differences in the diseases. These differences may be actionable. Mutational differences also suggest a future when clinicians may be positioned to better predict which ET and PV patients will progress. One confounding factor is the existence of a pre-fibrotic form of PMF that progresses to a fibrotic form of PMF; the differential diagnosis between this and ET is difficult and requires a an expert in these diseases. This is important as ET typically has a more indolent course, while pre-fibrotic PMF will likely progress to PMF, suggesting that more regular observations for pre-fibrotic PMF patients is warranted.
All MPNs may progress to other myeloid cancers, most commonly AML. This so-called “secondary AML” or “sAML” is much more lethal than de novo AML, which itself is usually lethal. The incidence of sAML is ~1% after 10 years for ET, ~2% for PV, and ~10-20% for PMF. There are some risk factors of progression, with slight variations between the different MPNs. Generally, older age, high number of platelets or white blood cells, blasts in the bone marrow, and chromosomal alterations are among the clinically observable manifestations of transformation. In addition, a number mutations are associated with leukemic transformation, including the epigenetic modifiers EZH2, ASXL1, IDH1, and IDH2, the mRNA splicing regulator SRSF2, and the tumor suppressor p53.
The only curative treatment for post MPN AML is hematopoietic stem cell transplant. Transplant patients do best when they first receive induction chemotherapy and receive a complete response. These patients may live for several years; however untreated patients may only survive for a few months.
LLS contributions
LLS-funded research led critical important contributions to our understanding of MPNs:
- In 2005, several groups simultaneously identified the JAK2 V617F mutation that is critical to many cases of MPNs. One group was led by Gary Gilliland, M.D., Ph.D. at the Fred Hutch Cancer Center who was funded through TRP. This was the first mutation described as being critical for, and specific to MPNs.
- In 2006, two collaborating groups identified mutations in MPL as contributing to MPN. One of these groups was led by Dr. Gary Gilliland, and newly independent Ross Levine M.D. (formerly a trainee in the Gilliland lab, now at the Memorial Sloan Kettering Cancer Center). This discovery represents the second leg of critical MPN mutations, and was funded by a TRP.
- In 2013, two groups identified neomorphic mutations in the calreticulin (CALR) gene. These mutations form the third leg of the critical genes for MPN. One group led by Anthony Green M.D. Ph.D. at the University of Cambridge in the UK was funded by a SCOR and published in the prestigious New England Journal of Medicine.
- In 2014 Scholar Ross Levine was the first to characterize the mutational spectrum of post-MPN AML, and identified p53 as a critical mutational target. His team further showed that combining a loss of p53 with the JAK2 V617F mutation leads to AML in a mouse model. This was the first model of post-MPN leukemic transformation.
- In 2019, the FDA approved the JAK2 inhibitor fedratinib for the treatment of myelofibrosis. This joins ruxolitinib, another JAK2 inhibitor for MF treatment. The advantage of having multiple drugs is that their precise mechanisms of action are different, and some patients may not tolerate ruxolitinib. This drug’s efficacy in mouse models of MPN was first reported in 2008 by Gary Gilliland’s team with support from TRP.