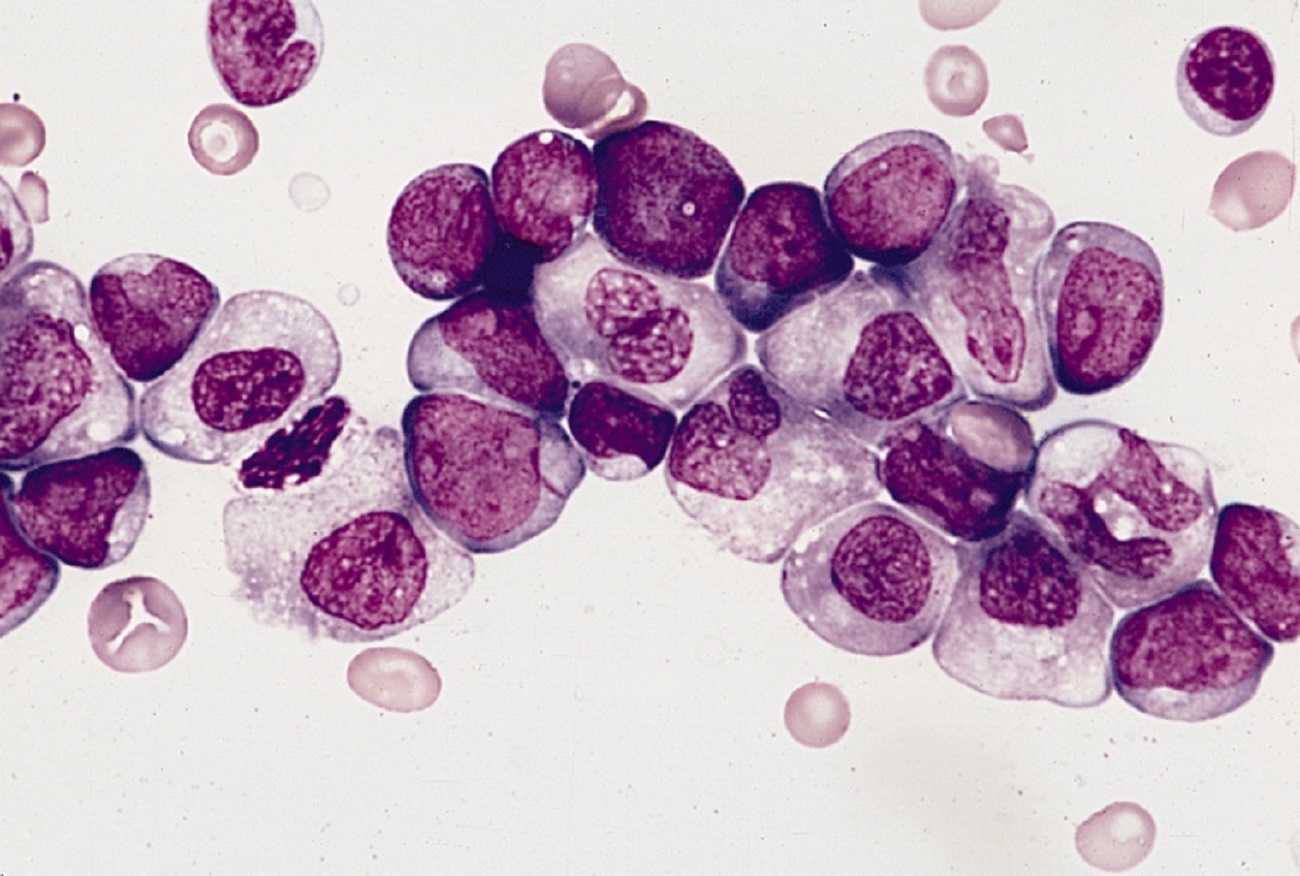
Acute myeloid leukemia (AML) is an aggressive, rapidly-progressing disease in which the immature blood cells do not develop properly and grow uncontrollably. The AML cells crowd out and interfere with the number and function of normal blood cells. The need for new treatments for AML remains urgent, which is why The Leukemia & Lymphoma Society (LLS) has invested approximately one quarter of its research dollars annually in the disease, more than $100 million over the past decade. This work is complemented by our Beat AML Master Clinical Trial that has been in progress since November 2016.
Despite the fact that AML is a rare cancer, occurring in about 20,000 new patients in the US per year, it represents approximately 10% of all new cases of blood cancer per year and 30% of all leukemias. Moreover, deaths due to AML is about 10,000 cases per year in the US, or 20% of all blood cancers.
Treatments for the disease can be curative for 50 percent or less in younger patients, who typically require aggressive cytotoxic chemotherapy and may also need a bone marrow transplant. However, long-term survival for older patients, who may ineligible for high dose chemotherapy or a bone marrow transplant, is poor. This is significant, since the average age for an AML patient is approximately 68 and, due to their age, cannot tolerate aggressive chemotherapy or a bone marrow transplant. It is estimated that in older patients, only 10% of patients will survive five years after diagnosis. At the other end of the spectrum, approximately 650 children develop AML per year in the US. While many children will be cured of AML with traditional cytotoxic chemotherapy and/or bone marrow transplants, those that do survive can have long-term side effects due to aggressive therapies, while urgent therapies are needed for those that fail chemotherapy.
Our understanding of the molecular basis for AML has dramatically improved over the past 10 years. This knowledge, along with technological improvements in new therapeutic approaches for cancer, is changing the outcome for patients. In fact, after a forty year drought of newly approved therapies for AML, the FDA approved 8 new drugs in the past two years to treat the disease and one to treat acute promyelocytic leukemia (APL), a subtype of AML. Of particular note, the combination of a new drug, venetoclax, combined with older standard cytotoxic therapy can provide long-term disease control for about 30% of newly diagnosed elderly patients with AML. Nevertheless, many newly diagnosed elderly patients treated with the venetoclax /azacitidine combination therapy simply fail to respond or will relapse. It is also very clear that childhood AML is molecularly distinct compared to adult AML and therefore is an opportunity to apply distinct, precision medicine for these children.
While we have begun to chip away at AML, there is still much more work to be done. LLS is supporting new research through close to 80 active academic grants to explore every avenue to further improve outcomes for AML patients. These efforts include:
- Precision Medicine: methods to quickly identify the patients’ molecular alterations (mutations) and develop novel therapies that specifically target those mutations;
- Activators of cell death: as the machinery that controls cell death have been identified, new approaches to activate cell death specifically in AML cells has been achieved. Venetoclax is one of these therapies, but other control mechanisms the mediate cell death are also in development
- Novel immunotherapies: such as activators of a family of AML-killer immune cells. Chimeric antigen receptor T-cell therapy (CAR-T) is one example (See below).
- Therapies that eliminate the so-called “leukemic stem cells” which are thought to be resistant to many current treatments and results in a disease relapse
- Regulators of master control molecular switches that are aberrant in AML
- Improvement in bone marrow transplants, which would make the procedure more effective without causing severe side effects.
- Safer cytotoxic therapies that have reduced side-effects and achieve equal or better outcomes compared to standard therapies.
- A special focus on pediatric AML designed to accelerate the use of experimental therapies for this subset of patients.
- Definition and identification of pre-leukemia with the anticipation that detecting and treating patients before they develop full blown leukemia will lead to better outcomes.
Are you a Patient or Caregiver? Click here for our free informational booklet on AML.
For detailed examples of how LLS is helping further AML Research, please read further.
Precision therapy
AML is actually a complex constellation of blood cancers, each driven by different molecular alterations. As advances in genomic technology have allowed researchers to better understand the underlying causes of cancer, the one-size-fits-all treatment of AML is giving way to more targeted approaches.
LLS is supporting multiple projects studying new agents with the potential to target specific mutations. The Beat AML Master Clinical Trial, an LLS-led collaboration, is testing multiple targeted therapies simultaneously at multiple cancer centers across the U.S. The trial is for newly diagnosed AML patients 60 and older. Patient bone marrow samples are analyzed to identify their subtype of disease so they can be matched with a targeted therapy for their mutation.
Exploiting Metabolic Vulnerabilities
Researchers have discovered that AML cells frequently display novel biochemical dependencies in which certain cellular processes and chemical reactions (termed “metabolism”) become increasingly important or critical for cancer growth. LLS is supporting a number of projects seeking to better understand these dependencies and develop novel therapeutic approaches that exploit these vulnerabilities. For example, Daisuke Nakada, Ph.D. (Baylor College of Medicine) has found that inhibition of a protein called AMPK, which regulates cellular utilization of nutrients, kills AML cells in model systems. Courtney Jones, Ph.D. (University of Colorado) has discovered that inhibiting usage of a key molecule (called nicotinamide), necessary for cell energy generation, selectively kills AML cells, particularly those found in relapsed disease. Adam Wilkinson, Ph.D. (Stanford University) is studying how uptake and breakdown of the amino acid valine plays a critical and specific role in the development of AML. Results from all of these and other studies will support the design and implementation of novel therapeutic approaches.
Cell Death Machinery
Just as cytotoxic drugs kill cells that are actively growing and replicating, it is also possible to tip the balance to push AML cells to death. LLS has invested over 20 years and $20 M of research into the development of venetoclax, which activates the cell death machinery. Andreas Strasser, Ph.D. (Walter and Eliza Hall Institute of Medical Research) and colleagues were pivotal identifying the mechanism of action of venetoclax. They have already identified some of the mechanisms that mediate resistance to venetoclax and are exploring new therapies to overcome resistance in novel clinical trials. Daniel Pollyea, M.D. (University of Colorado) and Maria Konopleva, M.D., Ph.D. (MD Anderson Cancer Center) have demonstrated that venetoclax in combination with cytotoxic agents, azacitidine or decitabine, produce dramatic and durable responses in some AML patients. The $5M collaborative team of Craig Jordan, Ph.D. (University of Colorado) has recently identified a unique AML cell type that is associated with resistance to venetoclax/azacitidine and likely to be distinct from that found by Dr. Strasser. Mala Shanmugam, Ph.D. (Emory University) has identified a biomarker to determine which patients may respond well to venetoclax. Loren Walensky, M.D., Ph.D. (Dana Farber Cancer Institute), is studying new therapies to inhibit pathways that control cell death in AML.
Immunotherapy
Immunotherapy is becoming a mainstay of many cancer treatments. Harnessing the body’s immune system is also being investigated in AML. Numerous ways to activate the immune system and enlist immune cells to kill tumor cells have been FDA-approved for solid tumors and some blood cancers. However, application of immune activators for AML still remains in the experimental stage. LLS support for directed immunotherapies includes Terry Fry, M.D. (University of Colorado) who is developing new CAR T cells specifically directing T-cells to AML tumor cells and killing such cells.
Targeting stem cells
Relapse in AML is very common and researchers suspect that minimal residual disease, small traces of cancer cells that remain after treatment, are one of the primary causes of relapse. Investigators are working to eliminate the AML cancer stem cells as a way to completely eradiate the cancer cells so the cancer does not return. This would be analogous to removing a tree at its roots compared to pruning the tree at its branches.
Craig Jordan, Ph.D. (University of Colorado) leads an LLS Specialized Center of Research team taking a multi-pronged approach to eradicate cancer stem cells in AML patients.
Regulators of Master Control Switches: Epigenetics
An area of cancer treatment known as epigenetics is focused on targeting the chemical changes that control cell behavior by switching genes on and off. Maria E. Figueroa, M.D., (Sylvester Comprehensive Cancer Center at Miami Health System), is working to understand why epigenetics go awry with age and lead to cancers like AML. Deeper understanding of these aberrations could lead the way to early intervention strategies, as some of the first changes in AML patients occur in epigenetic regulators. Jolanta Gremecka, M.D., (University of Michigan), who LLS previously funded to develop new epigenetic therapies now in the clinic for AML, is developing chemical agents to a new epigenetic inhibitor that is dysregulated AML.
Improvements in Bone Marrow Transplants
Allogeneic hematopoietic cell transplantation (alloHCT), a type of bone marrow transplant where the donor material comes from a normal patient and is placed into the AML patient, can be curative. However, one third of AML patients experience relapse and graft vs. host disease, where the body mounts an immune reaction to the donor cells, is a common life-threatening toxicity. Therefore, LLS is funding work to improve treatment outcomes. Katharine Hsu, M.D., (Memorial Sloan Kettering Cancer Center) is performing clinical studies to determine if selection of transplant donors with certain genetic markers predict for better transplant outcomes in AML patients.
Safer Cytotoxic Therapies
LLS was instrumental in supporting the work of a newly-approved cytotoxic therapy for AML, known as Vyxeos. This agent, which was approved by the FDA in 2017 for AML, appears to have better efficacy compared to conventional cytotoxic therapy. Kasey Leger, M.D., (Fred Hutchison Cancer Center) will work with a team of physicians to determine if Vyxeos has less cardiotoxicity compared to other AML therapies. This work is complemented by the investigation by Smita Bhatia, M.D. (University of Alabama) and Saro Armenian, D.O. (City of Hope) into the long term impact of anthracycline (a cytotoxic agent used in AML therapy) on cardiotoxicity in young adults who were treated for leukemia.
Pediatric AML Therapies
Approximately 650 new cases of pediatric AML occur each year in the US. It is estimated that 50% of those patients will be cured of AML with conventional cytotoxic therapies and alloHCT. It is now clear that genetic changes in pediatric AML are distinct from adult AML, and therefore new therapeutic targets and risk stratification methods will be needed for pediatric AML patients. LLS is funding the work of Soheil Meshinchi, M.D., Ph.D. (Fred Hutchison Cancer Research Center) to explore the use of an antibody conjugated to toxin for pediatric AML. The antibody is directed to mesothelin, which is highly and uniquely expressed in pediatric AML.
Other grants will focus on a particularly deadly mutation where mixed lineage leukemia (MLL) gene has been incorrectly fused to other genes. MLL- associated gene fusions are commonly found in infants with AML. Benjamin Garcia Ph.D. (University of Pennsylvania), Carolyn Felix M.D. (University of Pennsylvania), and Xiaobing Shi Ph.D. (Van Andel Institute), are studying new way to treat MLL-associated AML.
Scott Armstrong, M.D., Ph.D. (Dana Farber Cancer Institute) and Kevin Shannon, M.D. (University of California) are attempted to develop therapies that target so-called BET, which regulates epigenetic controls that drive pediatric AML.
Identification Pre-Leukemia Conditions
LLS has funded seminal studies done by Benjamin Ebert M.D., Ph.D. and colleagues (Dana-Farber Cancer Center) and Mark Minden, M.D., Ph.D. (Princess Margaret Cancer Center, Canada) who have shown that normal, healthy individuals have mutations in their blood that frequently are the same ones appear in patients with AML. In addition, the mutational load increases with age, such that 10% of individuals over 70 years of age have mutations in the blood. Moreover, such patients with mutations have a higher chance of developing AML. LLS is currently funding Liran Shlush, M.D., Ph.D. (Weizmann Institute of Science) to further explore this phenomena and attempt to develop relatively benign therapies to treat such “pre-leukemic” patients.
The LLS Therapy Acceleration Program and Ryvu Therapeutics (formerly known as Selvita) continue to collaborate to advance the novel agent SEL120, a drug that targets the protein known as cyclin-dependent kinase 8 (CDK8). CDK8 plays a unique and critical role in gene regulation and is implicated in the development of numerous hematological malignancies and solid tumors. SEL120 is an oral selective inhibitor of CDK8 and is currently in clinical development for the treatment of AML and high-risk MDS.
Image Copyright: The Armed Forces Institute of Pathology (AFIP) - PEIR Digital Library (Pathology image database).