The five-year survival rate for a child with leukemia 50 years ago was a dismal 3%, but with the advent of combination chemotherapy as standard of care in the 1960s, increasing understanding of the disease, and more recent discoveries of novel therapeutics, cures are now possible in children. LLS has been at the forefront in improving outcomes for patients with ALL. LLS supported pioneering work at the University of Pennsylvania, where researchers helped develop the first CAR T-cell immunotherapy for ALL, tisagenlecleucel, known commercially as Kymriah®, which attained approval from the U.S. Food and Drug Administration in 2017. There is still much work to be done and LLS is again leading the charge for ongoing and future work in the ALL landscape, both in pediatrics as well as in adults, where there remains tremendous unmet medical need.
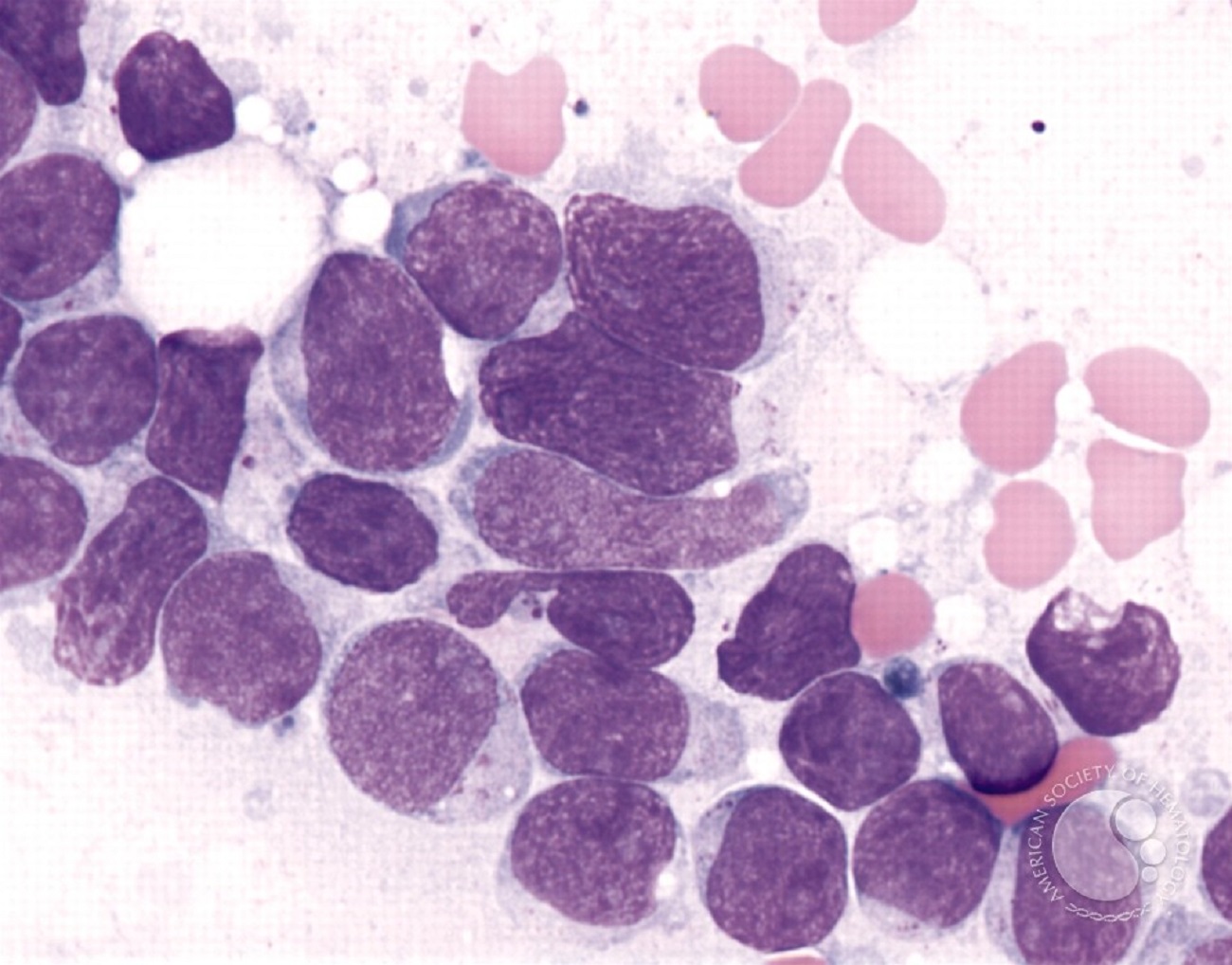
Acute lymphoblastic leukemia (ALL) is a malignant transformation and proliferation of white blood cells called lymphocytes. The hallmark of ALL involves chromosomal abnormalities and genetic alterations associated with differentiation and proliferation of the malignant cells. In 2019, it is estimated that approximately 6,000 new cases of ALL occurred in the US, which is less than 4% of all blood cancers. Roughly 50% of these ALL cases occur in children and represents greater than 30% of all pediatric cancers. The incidence of ALL follows a bimodal distribution, with the first peak occurring in childhood and a second peak occurring around the age of 50.
In children, survival rates for pediatric ALL have dramatically improved in the past 50 years, with cure rates exceeding 85% in children. However, resistance to therapy is common and for some children or adolescents many therapies simply do not work, resulting in the use of multiple rounds of alternative chemotherapy. Beyond this, the current therapies often lead to long term side effects (i.e. central nervous system impairment, cardiovascular issues, bone growth defects). Therefore, there is urgent need to develop safer, more effective treatments for ALL, particularly for children who are refractory or resistant.
In adults, despite advances in management, the backbone of frontline therapy remains multi-agent cytotoxic chemotherapy and for patients who can tolerate it, allogeneic (donor) stem cell transplantation. Elderly patients are often unable to tolerate such regimens and often face a particularly poor prognosis. Only approximately 30–40% of adult ALL patients achieve long-term remission.
Are you a Patient or Caregiver? Click here for our free informational booklet on ALL.
ALL can be classified into two main subtypes, B-cell acute lymphoblastic leukemia (B-ALL) and T-cell lymphoblastic leukemia (T-ALL). B-ALL s the most common subtype and occurs in immature cells that would normally develop into B-cells, important for immunity. B-ALL is more common in children, constituting approximately 88 percent of cases, whereas in adults, B-ALL represents about 75 percent of cases. T-ALL is less common, occurs more often in adults than in children, and originates in immature cells that would normally develop into T-cells, important for fighting infections. Novel therapies for T-ALL in particular are lacking and represent a critical unmet clinical need.
In addition to classifying ALL as either B-ALL or T-ALL, further classification can be based on changes to certain chromosomes and genes. Although both children and adults experience the same types of cancers, it is now well established that pediatric and adult B-ALL have different molecular profiles. About 25 percent of adults and about 3 percent of children have an ALL subtype called “Ph-positive ALL” (“Ph+”). In Ph+ ALL, a translocation between chromosomes 9 and 22 leads to the abnormal BCR-ABL fusion gene that makes an abnormal protein that helps leukemia cells to grow. Tyrosine kinase inhibitors (TKIs) are used to treat Ph+ ALL by blocking the BCR-ABL protein from sending signals that cause leukemia cells to form. Recently, genomic profiling has established a Ph-like ALL phenotype that is particularly prevalent in children with a high-risk of relapse and poor survival, but no agents have been approved in this setting yet. The following TKIs are approved to treat Ph+ ALL:
- imatinib (Gleevec®) – adults with relapsed or refractory Ph+ ALL & children with newly diagnosed Ph+ ALL in combination with chemotherapy
- dasatinib (Sprycel®) – adults with Ph+ ALL with resistance or intolerance to prior therapy & children with newly diagnosed Ph+ ALL in combination with chemotherapy
- ponatinib (Iclusig®) – adult patients with T315I-positive Ph+ ALL, where T351I is a specific mutation that occurs in the BCR-ABL protein leading to resistance to imatinib and dasatinib
While 5-year survival in pediatric ALL has increased steadily over the years, certain subtypes of pediatric ALL have no adequate cures. The treatment regimens for ALL usually include a cocktail of cytotoxic chemotherapy agents, as well as a bone marrow transplant if patients are deemed qualified to tolerate the therapy. Strikingly, over the past few decades, there have been only a limited number of new non-chemotherapy treatments approved for use in pediatric ALL (blinatumomab, a therapy in a category known as bispecific T-cell engager (BiTE), and tisagenlecleucel); and in adult ALL (blinatumomab and inotuzumab ozogamicin, an antobidy therapy linked with a cytoxic therapy). New drugs are needed to improve the outcome of adult ALL and for those pediatric ALL patients who do not respond to frontline therapy.
The FDA has approved the following drugs for relapsed and/or refractory ALL patients:
- tisagenlecleucel (Kymriah®) – children with refractory B-ALL or have had two relapses (click here for further information)
- inotuzumab ozogamicin (Besponsa®) – adults with relapsed or refractory B-ALL
- blinatumomab (Blincyto®) – adults with relapsed or refractory B-ALL; adults and children with B-ALL in remission but have still not achieved minimal residual disease (MRD), meaning no trace of cancer cells are detectable.
- liposomal vincristine (Marqibo®) – chemotherapy for adults with relapsed Ph-negative ALL
- nelarabine (Arranon®) – adults and children with relapsed T-ALL
- asparaginase Erwinia chrysanthemi (Erwinase®) – ALL patients with hypersensitivity to E-coli-derived asparaginase, which is the standard of care as part of a chemotherapy regimen
- clofarabine (Clolar®) – children with relapsed or refractory ALL
There is still much more work to be done for the treatment of ALL. LLS is currently supporting new research through 26 active academic grants to explore every avenue to further improve outcomes for ALL patients. In FY19, ALL research accounted for approximately 5% of the annual research dollars spent by LLS. This is approximately $2.5 million associated with a $6.7 M commitment over 3-5 years. A plan has been implemented at LLS to significantly increase the funding for pediatric blood cancers (which principally includes ALL and acute myeloid leukemia (AML). In July 2019 nine new grants in ALL were activated, with seven of them focused on pediatric ALL). In fiscal year 2019 we have increased the overall pediatric blood cancer research funding by 200-300%. Two new grants in ALL are from the newly initiated Blood Cancer Discoveries Grant Program that launched in July 2020.
For detailed examples of how LLS is helping further ALL Research, please read further.
Discovering Novel Targets and New Therapies in B-ALL
Jerry Chipuk, Ph.D., (Icahn School of Medicine at Mount Sinai) recently identified that dynamin related protein 1 (DRP1)-dependent mitochondrial fission is required for RAS-induced cellular transformation. He proposes to investigate how DRP1 governs leukemia cell survival and chemotherapeutic responses using state-of-the-art imaging, metabolomics, and apoptosis techniques with cellular models and ex vivo leukemia patient samples to ultimately determine whether DRP1 is a novel druggable target to kill leukemia cells.
Novel Targets and Pathways in T-ALL
The developmental landscape of T-ALL is ripe for further exploration. LLS is funding a number of grants that delve into the novel pathways of this disease and look to better understand how the disease is driven while also developing novel therapeutics. For example, David Teachey, M.D., at the Children’s Hospital of Philadelphia is exploring daratumumab, FDA approved for myeloma, for use in pediatric T-ALL. T-ALL has a predilection for infiltrating the central nervous system (CNS). All children diagnosed with T-ALL receive CNS-directed chemotherapy, with the potential for lasting neurological toxicity. CNS relapse nonetheless occurs in 3-8% of ALL patients, with a higher risk in T-ALL. Because the requirements for T-ALL to enter and survive in the CNS remain unknown, no alternative therapies are available. Susan Schwab, Ph.D., (New York University) will use a multi-pronged approach to understand CNS accumulation and more generally how T-ALL colonizes the CNS.
Overcoming Resistance in ALL
Response patterns to blinatumomab, a type of antibody therapy that forms a bridge between the cytotocix T cells and the tumor cells, are essentially binary, with some patients having a striking response, and others showing no response at all, despite adequate expression of the targeted protein, CD19, on the leukemia cells. Patrick Brown, M.D., at Johns Hopkins University is studying immunologic basis of response and resistance to blinatumomab in pediatric and young adults with relapsed B-ALL. Additionally, a specific recurrent mutation of NSD2 has been identified in childhood ALL, particularly in relapsed patients. Jianping Li, M.D., at the University of Florida, is exploring the spectrum of therapy resistance conferred by NSD2 mutation, using mouse models to determine the molecular mechanism of therapy resistance of ALL cells. Unlike in myeloid leukemia, approaches to eradicate the leukemia initiating cells (LIC) in B-ALL remain elusive. For this reason, Markus Muschen, M.D., Ph.D., (City of Hope) will develop therapeutic approaches to target rare LIC in B-ALL, as successful targeting of LICs in other diseases have helped improve outcomes by reducing the risk of drug-resistance and relapse and overall toxicity and side-effects.
Novel and Safer Chimeric Antigen Receptor (CAR) T Cell Immunotherapy Approaches
While CAR-T cells have emerged as a promising treatment for relapsed/refractory ALL, but for some patients the CAR-T cells fail to persist, resulting in leukemia relapse and poor durable remission. Barbara Savoldo, M.D. at the University of North Carolina is conducting a clinical trial to determine if an improved version of CAR-T can be safely administered to adult and pediatric subjects with relapsed/refractory ALL. Additionally, Ryotaro Nakamura, M.D., at the Beckman Research Institute of the City of Hope proposes a novel approach to improve efficacy and durability and expansion of CAR T cells using properties of cytomegalovirus (CMV)-specific T cells and a novel CMV vaccine. He will evaluate safety, persistence/expansion of CMV-CD19 CAR T cells, and clinical efficacy in ALL patients undergoing a hematopoietic stem cell transplant.
Mixed-lineage Leukemia (MLL)
MLL defects occur in 70% and 10% of infants and adults, respectively, with ALL. Rearrangements to the MLL gene result in some of the most aggressive leukemias in both children and adults. A number of LLS grantees will explore the novel targets in MLL leukemias: Dot1L by Carolyn Felix, M.D., at the Children’s Hospital of Philadelphia and Dpy30 by Hao Jiang, M.D. at the University of Virginia.
Identify novel genetic subtypes of B-other ALL
A significant proportion of B-ALL cases (10-30%) cannot be classified into traditional subgroups as well as have poor outcomes. Zhaohui Gu, M.D., at St. Jude Children's Research Hospital will explore cases caused by recurrent genetic alterations or commonly disturbed pathways to better characterize these genetic subtypes.
Relapse prediction
Relapse prediction is being explored by Rong Lu, Ph.D., working at the University of Southern California, where he will analyze individual human ALL cells from initial diagnosis and relapse stages of the same patients using a mouse xenotransplantation model, and analyze chemo response at the cellular and molecular levels. He aims to identify the key cellular and molecular events that drive leukemia genesis and relapse.
Ph-like ALL (BCR-ABL1 like)
This subtype comprises up to 25% of B-ALL and is characterized by a diverse range of genetic alterations activating kinase signaling pathways and poor outcome. While ABL and JAK inhibitors have entered clinical trials of Ph-like ALL, there is preclinical and clinical evidence that CRLF2-rearranged Ph-like ALL, which accounts for over half of cases, will be poorly responsive. Charles Mullighan, M.D., at St. Jude Children's Research Hospital, aims to develop and test the activity of JAK2-directed protein degradation using proteolysis-targeting chimeras (PROTACs) in CRLF2-rearranged Ph-like ALL models.
The image was originally published in ASH Image Bank. Peter Maslak. Precursor T-cell Acute Lymphoblastic Leukemia. ASH Image Bank. 2003;2281 © the American Society of Hematology.