Follicular lymphoma (FL) is derived from white blood cells that grow in an uncontrolled, slow manner. Therefore, FL is considered an indolent disease that may require treatment. FL is the most common slow-growing non-Hodgkin's lymphoma. To date, although this slowly progressing disease can be managed, reoccurrence of the disease is common and therefore, new treatments are needed. FL has an annual incidence of about 15,000 cases/year in the United States with patients having an average age of approximately 60. The five-year-survival-rate is 87.7%, with younger patients having a higher survival rate. LLS has supported research leading to most of the therapies in use for FL, and is currently supporting novel approaches to treatment the disease, particularly through immunotherapy. Diagnostic evaluation of the potential FL patient is critically important, as that this will determine the treatment for the disease. In general, the physical exam, lymph node biopsy with pathological evaluation, bone marrow biopsy, as well as whole body imaging will provide the key information to make the definitive diagnosis, prognosis, and treatment plan.
Are you a Patient or Caregiver? Click here for our free informational booklet on non-Hodgkin's lymphomas.
Treatments and the Need for Further Research
The treatment for FL depends on the grade of the disease. Because of the indolent nature of the disease, and since progression can be slow, a watchful waiting approach may be appropriate in patients with limited tumor burden and little to no clinical symptoms. In some cases of early stage FL, radiation may be curative in 40-50% of patient. However, because of the indolent nature of the disease that are without overt symptoms, few patients present with early-stage disease, and therefore most FL patients require further therapy. Beyond this, a low percentage of patients with FL will transform to an aggressive lymphoma.
At this time it is impossible to predict with good certainty if and when patients will develop more advanced disease or respond well to therapy. The main focus of FL-research is to:
- understand the causes and evolution of the disease
- develop better diagnostic methods using molecular methods to detect early disease or relapse
- understand why our existing treatments work and often fail to work well and
- develop better therapies to overcome resistance or completely new therapies that avoid resistance and/or complement our existing therapies.
Good progress has been made, but much more work is still needed.
Current therapy and its limitations:
A) Treatment options for newly diagnosed patients
The standard of care for a newly diagnosed, stage III/IV FL patient presenting with at least 1 high grade tumor burden criteria is cytotoxic therapy combined with a CD20 antibody known as rituximab (R). The exact components of the cytotoxic therapy can vary, but typically they consist of cyclophosphamide, doxorubicin, vincristine, and prednisone. The abbreviation for this therapy is known as R-CHOP. Another common alternative is to use the cytotoxic agent known as bendamustine plus rituximab (BR). Replacement of rituximab with obinutuzumab (a more powerful form of rituximab) in R-CHOP or BR therapy may further improve progression-free survival.
While over 90% of patients treated with R-CHOP will experience significant tumor shrinkage, and approximately 50% of patients will not have disease progression 10 years after therapy, these therapies have significant limitation. First, the therapies are not curative and relapsed disease is expected. Second, patients develop resistance to the therapies and therefore, new therapies that do not inhibit the same cellular machinery as the first therapy may be needed. Third, these therapies have major short-term, transient side effects (i.e. hair loss, fatigue) as well as long term side effects. For example, patients treated with R-CHOP or other cytotoxic agents have an increased risk of leukemia and cardiovascular disease due to exposure of cytotoxic drug in the R-CHOP cocktail.
B) Treatment options for patients with relapsed disease
Within the past few years, two types of therapies have been approved by the FDA for R/R FL. In almost 50% of patients, the therapies will include retreatment with a CD20-directed therapy (i.e. re-exposure to rituximab). For example, FDA recently approved the use of lenalidomide (an immune activator) plus rituximab (known as R2) in R/R FL patients. This combination produces superior efficacy compared to R alone (with 3 year progression free survival), Other FDA-approved alternatives include the use of PI3K inhibitors known as copanlisib, idelalisib, or duvelisib, which can be used after patient fail two or more therapies. PI3K inhibitors can induce progression-free survival for approximately 1 year. LLS supported early work that led to the discovery and development of PI3K inhibitors, and continues to fund work to explore the basis of resistance to such drugs.
Numerous experimental therapies are in development and hold great promise to further extending the disease-free interval in FL patients. The most notable results have been obtained with new immunotherapies and comes out of ground-breaking work supported for over 30 year by LLS (well over $100 M spent to date), which shows that reactivation of the immune system can control many types of hematological diseases including patients with R/R FL.
One class of new antibodies are known as bi-specific antibodies. These antibodies bind to CD20 on the surface of the tumor cells and CD3 on the surface of the T-cell (a component of the immune system). When the T-cell comes in contact with the tumor cell, it can kill the malignant cell. Three bispecific antibodies of this type induce significant tumor shrinkage in about 40-70% of patients, and about 50% of patients have no detectable tumor by radiographic methods. The duration of the antitumor activity is still under evaluation. Other immunotherapies, including the use of a so-called CD47 antibody plus rituximab induce high response rates. Discovery of the CD47 antibody was supported by LLS through our grant mechanism, as is clinical development of this combination to this day via the LLS Therapy Acceleration Program. In addition, it has recently been reported that chimeric antigen receptor –T cell therapy (CAR-T) has demonstrated efficacy in R/R FL patients. In this therapy, T-cells are obtained from the patient, genetically engineered to recognize the FL cells in the manufacturing site, and re-infused back into the patients, usually as a single dose therapy. LLS played a pivotal role in the development of CAR T therapy since its rudimentary development in the 1990’s to its approval in 2017. Our prior support exceeds $80 M. We continue to support improvements to CAR T therapy and immunotherapies in general.
Precision medicine, which targets a mutation in FL, is also being explored for relapse/refractory FL. One example is the use of tazometastat. Tazometastat is an oral medication that preferentially targets a gene known as EZH2, which controls a process known as epigenetics or gene expression. EZH2 is mutated in approximately 25% of FL patients. In relapsed / refractory FL patients with mutated and normal EZH2, tazometastat induces responses in approximately 70 and 35% and progression free survival is approximately 11 and 6 months, respectively. LLS supported work to discover this mutation in FL patients and continues to support new uses of EZH2 inhibitors through our academic grant program.
C) Treatment options for transformed FL (tFL)
It is estimated that approximately 2% of FL patients per year will transform from a FL to a more aggressive lymphoma (called tFL). tFL has similar properties to DLBCL, another aggressive lymphoma. While the median overall survival following transformation can be up to approximately 4 years, those patients that undergo early transformation after initial diagnosis have a worse outcome. The most common treatment for tFL is R-CHOP that can be followed by autologous stem cell transplantation. Patients with transformed FL (tFL) can also be treated with CD19 CAR T therapy where high overall response rates have been reported in the 16 patients included in this study (see DLBCL summary sheet). Responses have also been reported with bi-specific antibodies.
The Future of FL Therapy and Research
There is still much to be learned about FL especially since the disease is still considered incurable. This will require intensive laboratory investigation and clinical trials. LLS is supporting both strategies through over a dozen grants to academic institutions and two Therapy Acceleration Program partnerships with biotechnology companies. LLS’ total commitment to this area is approximately $25 M over the next 3 years. Beyond this, LLS brings to bear its 200 active grant programs (greater than a $200 M commitment) in blood cancers, many of which have relevance to treating lymphoid malignancies. For example, LLS has supported the foundational development of the 47 monoclonal Ab, venetoclax, ibrutinib, and CAR T; all of these are being applied to FL patients but none of which were initially developed for the treatment of FL.
Most notably, LLS is supporting work to fully understand the mutations that occur in FL patients (there are many) and which mutations cause the disease. In addition, it is now clear that the immune environment that surrounds the malignant cell may be just as important driving the disease as the mutations in the tumor cells themselves. This has immediate therapeutic implications and has led to new therapies deploying CAR T cells and anti-CD47 antibodies; both efforts have been extensively supported by LLS during the past and current funding efforts.
The key research priorities for LLS in Follicular Lymphoma:
- Identify the 2% of FL patients who are more likely to transform to an aggressive lymphoma and develop better therapies for these patients.
- Understand the basis or resistance to existing therapies and develop new therapeutic strategies to avoid resistance, take advantage of it, as well as develop new therapies that avoid resistance or can be combined with other therapies to kill FL tumor cells synergistically.
- Understand the evolution of follicular lymphoma from a common progenitor cell (i.e. cell of origin) to full follicular lymphoma.
- Develop and evaluate the use of circulating tumor DNA (ctDNA ; a liquid biopsy from the blood), which may better define the individual patient’s tumor heterogeneity and the identification of rare clones that impact the disease trajectory. ctDNA could provide a reliable index to determine when to stop and start therapy well before a radiological response is detected.
- Enroll patients who progress early or have other high-risk features in a clinical trial assessing novel treatment approaches. (Deprioritize clinical trials that attempt to improve therapy for low-risk patients).
- Define the role of the microenvironment in laboratory studies, including correlative studies in ongoing clinical trials, to best inform clinical trial design and endpoint analysis in future clinical trials of agents that affect the microenvironment.
- Further define the role of epigenetic mutations in FL (including EZH2 mutations) and use this information to inform clinical trials using these agents.
- Further understand the microenvironment and immune environment of FL to identify novel immunotherapy approaches, including CAR T, bispecific antibodies, checkpoint inhibitors, or vaccines, which may target FL cells as well as overcome an immunosuppressive microenvironment.
- Develop and apply reliable quality of life measurements to characterize the performance of therapies, especially in low-risk patients who are likely die of other causes. Incorporate these tools in the clinical assessment of novel therapeutic approaches for FL.
- Understand the defects in that control cell death in FL patients and apply novel therapies that control cell death (known as apoptosis) such as venetoclax, which is FDA approved for other blood cancers.
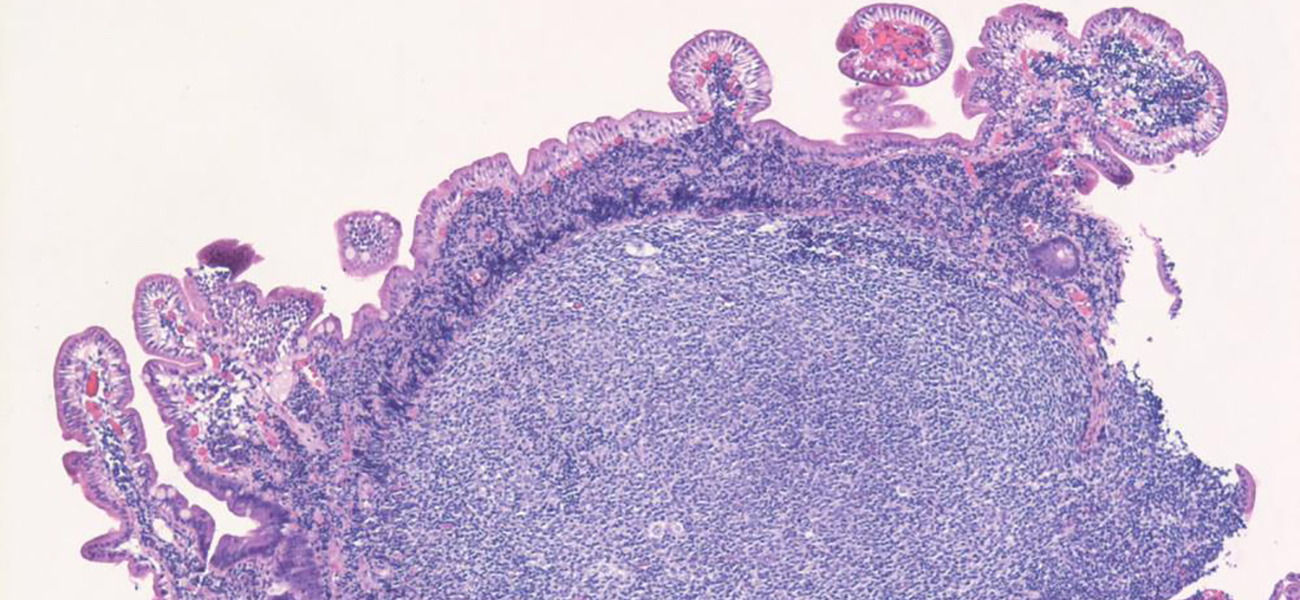
The image was originally published in ASH Image Bank. Girish Venkataraman, MD, MBBS. Duodenal follicular lymphoma. ASH Image Bank. 2020;61533. © the American Society of Hematology.