Outcomes for the treatment of chronic myeloid leukemia (CML) have dramatically improved over the past 50 years. While the ten year survival rates were less than 20% with the use of cytotoxic agents in the 1970’s, and improved to 50% with bone marrow transplants, the biggest improvements occurred within the last 20 years after the approval of an oral therapy, known as imatinib.
Today, the ten year survival rate for the most common form of CML is approximately 85% and patients can expect to live life-spans nearly as long as normal healthy adults.
Early support from LLS that has led to the development of imatinib made this happen.
Are you a Patient or Caregiver? Click here for our free informational booklet on CML.
The rise of precision medicine for patients with CML
Imatinib (Gleevec®), supported by LLS, changed the outlook for CML patients, turning a once fatal diagnosis into a manageable condition for most patients. It has saved an estimated 350,000 lives globally since its approval by the U.S. Food and Drug Administration (FDA) in 2001 and is now approved for more than 10 indications, including stomach and skin cancers. Imatinib launched a new class of drugs called tyrosine kinase inhibitors (TKIs) – the first targeted therapies developed for cancer.
The journey to develop imatinib took more than a decade and involved researchers from around the world. Funding from LLS provided critical support at key progress points, from the discovery of a genetic abnormality, known as the Philadephlia chromosome, by Janet Rowley, M.D. at the University of Chicago, to visionary proof of concept work by Brian Druker, M.D., Director of The Knight Cancer Institute at Oregon Health & Science University (OHSU).
With LLS support, Dr. Druker found a way to “turn off” the kinase enzyme, paving the way for targeted therapy, a cornerstone of precision medicine. Today, more than 40 kinase inhibitors are approved to treat other cancers, including breast, lung, kidney and colon cancer. Dr. Druker played an instrumental role in transforming care for patients with CML and continues to drive innovation in precision medicine through our Beat AML® Master Clinical Trial.
Newer, second generation TKIs further expanded the treatment armamentarium for CML. Following imatinib, the FDA approved three TKIs for use in the frontline setting: nilotinib (Tasigna®), dasatinib (Sprycel®) and bosutinib (Bosulif®), all advanced with LLS support somewhere along their development journey. Notably, imatinib, nilotinib and dasatinib are approved to treat pediatric patients with CML. CML is rare in children, accounting for about 3 percent of all newly diagnosed childhood leukemias, and treatment often follows guidelines developed for adults despite differences in disease biology and progression. More pediatric research studies are needed to evaluate the use of TKI therapy in children with CML. Beyond this, the Philadelphia chromosomal abnormality or a Philadephia-“like” abnormality is found in some children with acute lymphoblastic leukemia (ALL) and imatinib as well as other related TKIs have been used to effectively treat ALL with this abnormality.
While we’ve made significant progress, challenges remain. That’s why LLS continues to invest in the most promising CML research.
Imatinib is not effective for all patients, and all TKIs have potentially serious side effects. What’s more, these treatments do not often eradicate CML, and many patients need to stay on therapy indefinitely or risk disease progression. Nevertheless, we have discovered that some patients can stop taking TKIs without having the disease return for as long as we have monitored them.
On the research front, the greatest needs are improved diagnostics that accurately determine optimal treatment; knowledge of “deep remission,” which will allow more patients to safely stop therapy; and treatments that target the cancer stem cells, thereby completely eradicating the disease and eliminating pathways for recurrence or progression.
Here’s how LLS is addressing these needs through our support of cutting edge research:
Amer Zeidan, MBBS at Yale University, is combining TKIs with a drug that targets the PD-1 checkpoint protein on immune system T-cells. Research suggests that patient relapse might be due to the inability of the immune system to control remaining CML cells in the body. By augmenting TKIs with an immune checkpoint inhibitor, Dr. Zeidan is working to improve treatment for CML patients with minimal residual disease. His goal is eradication of the disease, without the need for a lifetime of continued treatment.
Timothy Hughes, M.D., MBBS, FRACP, FRCPA at the South Australian Health & Medical Research Institute, recently focused on optimizing therapeutic protocols earlier in a patient’s treatment cycle. Dr. Hughes and his team have mapped predictive assays, which measure the type and level of genes that are active in a patient’s leukemic cells at diagnosis and after initial therapy, as well as the range of cancer-associated proteins present in the plasma at diagnosis. Dr. Hughes is developing these assays into an easy-to-use format for clinical use to help identify patients who may be less responsive to initial therapy for CML and need more aggressive therapy and follow up while on TKIs.
Looking to the future: a new paradigm
Thanks to treatment breakthroughs pioneered with LLS support, patients with CML can expect a similar lifespan to the general population. Now, the treatment landscape is evolving to focus on treatment-free remission and identifying those patients who are high risk at time of initial diagnosis. In addition, LLS is helping to explore how the immune system can be recruited to further enhance therapy for CML patients. LLS is at the forefront of precision medicine and will continue to accelerate impactful research to improve the quality of life of patients with CML and help make long-term, treatment-free remission a reality for more patients.
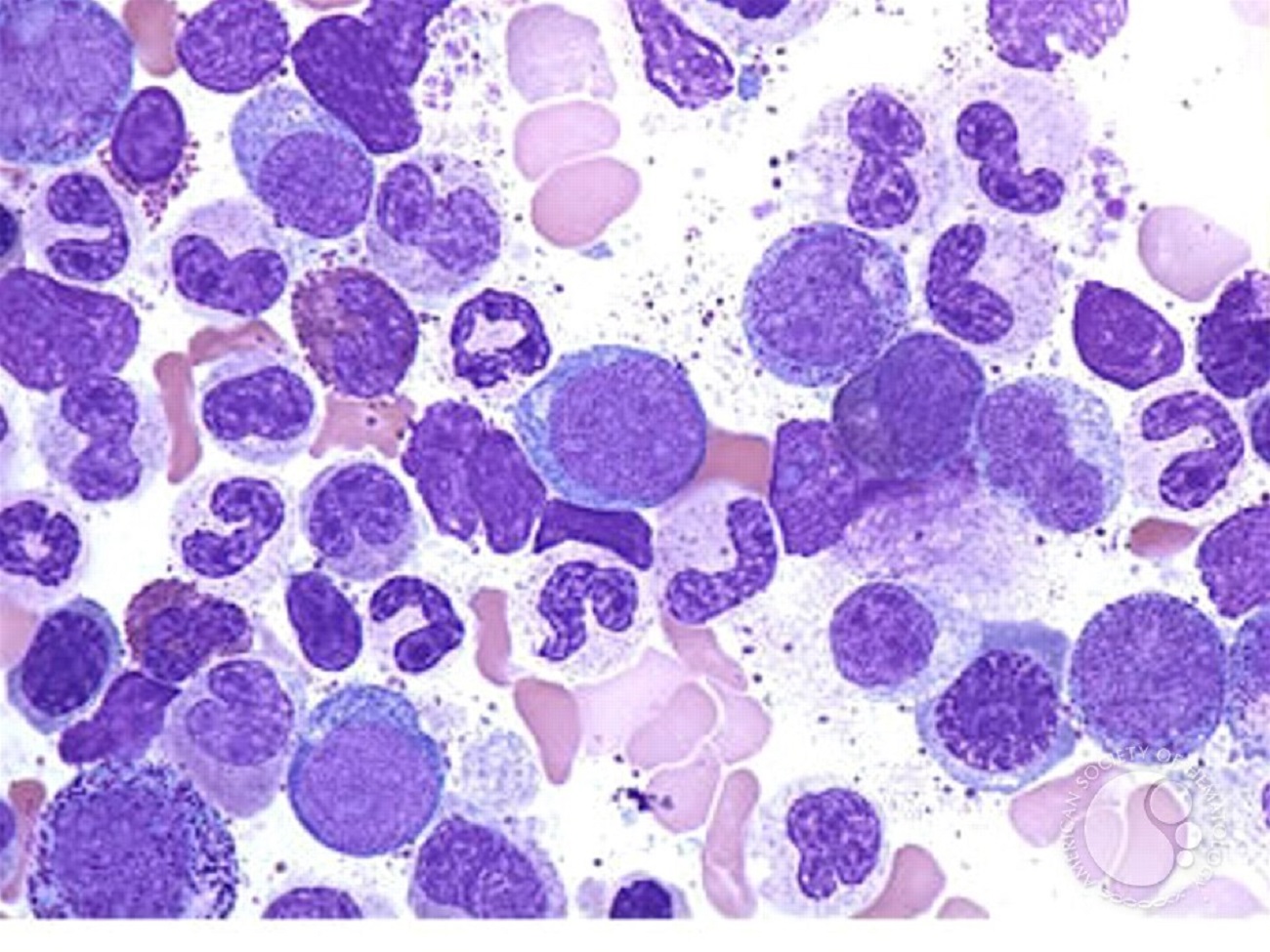
The image was originally published in ASH Image Bank. Peter Maslak. Accelerated Phase CML. ASH Image Bank. 2004;2394. © the American Society of Hematology.